Creighton News

News Contact
Casey Hoag
Senior Director,
External Communications
caseyhoag@creighton.edu
206.947.7778
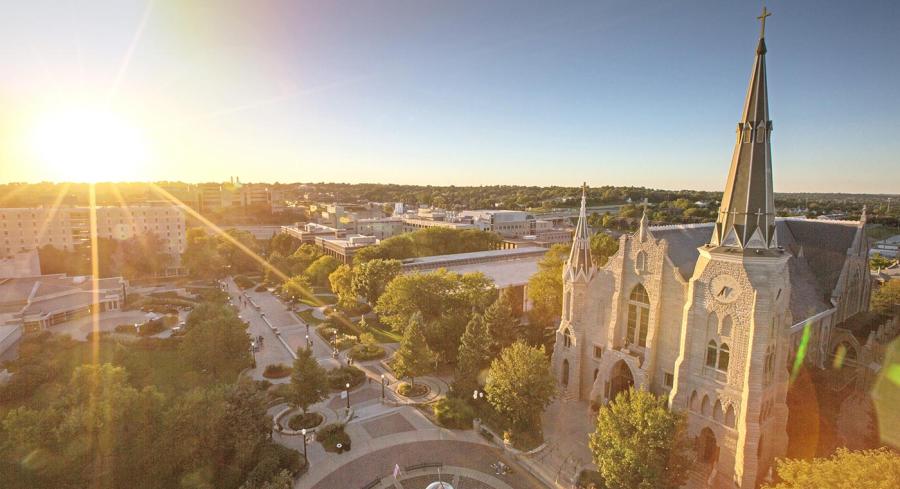
A Jesuit, Catholic University since 1878
Creighton University is a Jesuit, Catholic university bridging health, law, business and the arts and sciences for a more just world.
University Communications & Marketing
2500 California Plaza | Omaha, NE 68178